What is Hypermobility?
Hypermobility is generally regarded as the greater-than-average range of motion of the body’s joints. It can exist on its own in one or more specific joints or impact the whole body, and it can be a feature of two syndromes: hypermobile Ehlers Danlos Syndrome (hEDS) and Hypermobile Spectrum Disorder (HSD). So, what’s the difference?
Generalized joint hypermobility occurs when many joints throughout the body are considered hypermobile, with localized joint hypermobility occuring in one joint or group of joints in the same area. Joint hypermobility can be acquired through injury or it can be genetic, and it can present with or without joint instability and with or without accompanying symptoms. Hypermobile joints that are also unstable can experience subluxations, dislocations, sprains, tears, pain, and other injuries.
Hypermobile Ehlers Danlos Syndrome, or hEDS, is the most common subtype of a total of 13 types of the Ehlers Danlos Syndromes–while each subtype impacts the body differently, the root issue stems back to the body’s connective tissue. Connective tissue and its main component, collagen, is the glue that holds the body together– it is responsible for elasticity, strength, and stability. Without properly functioning connective tissue, the body can experience joint hypermobility and instability, pain, and fragility of the tissue itself.
The hypermobile type of EDS is the most common subtype–while research once suggested it occurs in 1 of every 5000 people, new research suggests that it is closer to 1 in every 500. This suggests that hEDS is not necessarily rare, but rarely diagnosed–that said, the other 12 subtypes of EDS do seem to be rare.
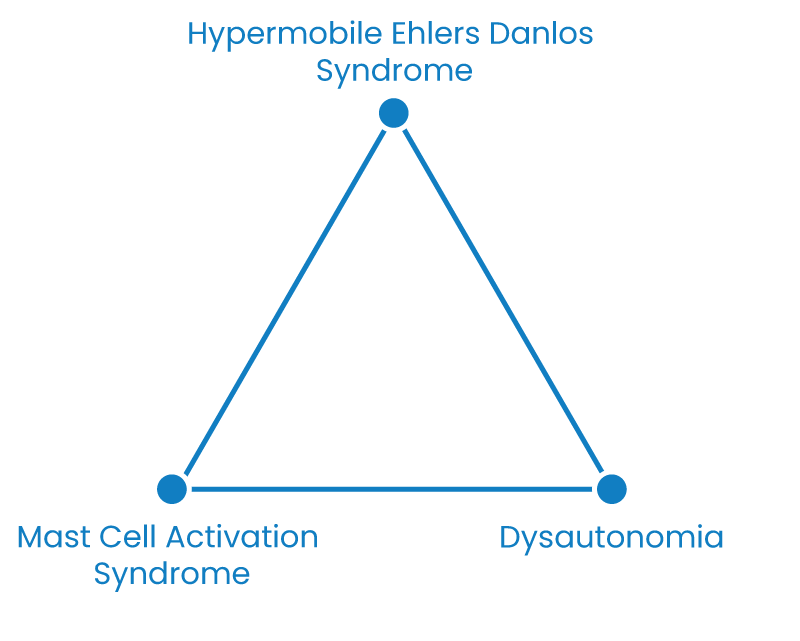
Hypermobile Ehlers Danlos Syndrome can present with comorbidities such as dysautonomia (disruption of the body’s autonomic nervous system) and/or mast cell activation syndrome (overactivity of histamine production by the body’s mast cells, creating allergic reactions to a variety of stimuli), commonly referred to as the “trifecta.” Both of these comorbidities point to a shared root cause of the body struggling to regulate its nervous system.
While EDS is a genetic condition, the genetic marker specifically for the hypermobile type has not yet been identified. As such, it is diagnosed clinically via a set of diagnostic criteria. Those who have symptomatic joint hypermobility but do not meet the full criteria for hEDS may instead be diagnosed with Hypermobile Spectrum Disorder. That said, treatment of both hEDS and HSD is essentially the same, particularly as knowledge and research around both syndromes continues to develop.
It’s worth noting that, while the increased range of motion of hypermobility can also mean increased flexibility, many hypermobile folks experience a lack of flexibility from muscles that tighten to try and stabilize loose joints. This is important when considering the impact of hypermobility on the musician, as well as managing the balance between strengthening muscles to help stabilize joints while also treating any pain or tension that arises. It’s also worth noting that there are other connective tissue disorders for which hypermobility can be a feature, including Marfan Syndrome.